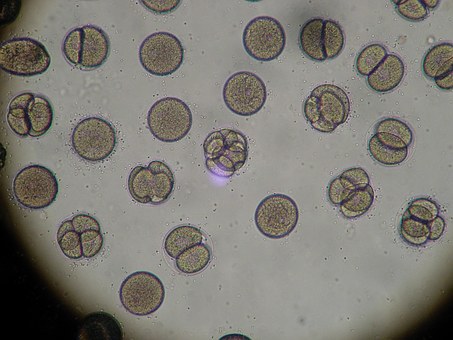
Mold and its Role in Allergic Fungal Sinusitis
Hallmarks of Allergic Fungal Sinusitis are nasal polyps fleshy outgrowths from the lining of either the nasal passages or sinus cavities. These are the result of chronic inflammatory changes. Another finding associated with AFS is the thick consistency of the mucous AFS produces. Terms such as peanut butter and axle grease have been used to describe the type of mucus found in sufferers of AFS. Patients that do have AFS are prone to developing secondary bacterial infections. All of us are normally colonized with bacteria in our sinus cavities but we’re not all walking around with sinus infections.
According to the medical literature, it is believed that 5-10% of the patients with chronic sinusitis suffer from AFS. My clinical experience leads me to believe that the incidence is much higher, especially in high-risk areas like the Southeast which has tremendous vegetation, high humidity and mild winters. Basically all the things necessary for mold to thrive. It’s not unusual for me to have patients who grew up in the frigid North or the dry Southwest who never had sinus issues become chronic sinusitis sufferers when they moved to where I’m located in the greater Atlanta area. Few have the ability to relocate back to sinus friendly environments and live happily ever after at least from a sinus point of view. Unfortunately many do not have the luxury of moving and suffer for years before the proper diagnosis is made.
One reason why Allergic Fungal Sinusitis may be missed is that mold may not be easily cultured using conventional methods. Also in milder cases, clinicians may not see polyps or thick peanut butter type mucous and only see that the lining appears inflamed. Better methods of testing are needed and there is one company interested in working with me on this looking more for the genetic footprint of the mold rather than trying to grow it by conventional methods. Until then clinicians must rely on the tried and true method of history taking. It amazing what can be learned from a patient if you just listen. Unfortunately, as we move more towards point and click medicine history taking is becoming a dying art.
Steroids have been used to treat AFS but like those that respond to antibiotics many patients with AFS relapse once the steroids are stopped. Today the hallmark of treating AFS is with antifungals. The easiest way to deliver the antifungals to the sinus cavities is to have them aerosolized mechanically this can be used alone but more likely in combination with antibiotics, steroids and possibly agents known as mucolytics to break mucous and biofilms which may prevent the medication from reaching their targets. All of these medications can be delivered through nebulizers and atomizers minimizing many of the side effects when they are taking orally. For a patient with milder disease, this is the ideal way to treat, testimonial by Justin.
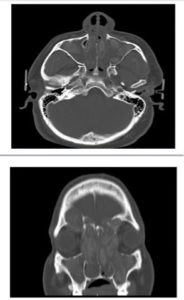 However, for patients with more extensive disease, Clazon Martin CT scan (on right), such as the patient whose CT scan saw his disease was so extensive that the polyps were causing his Left eye to bulge out, oral or intravenous antifungals may be necessary. This should not be taken lightly and should be managed by someone such as an infectious disease specialist to be done safely. Once these more severe cases improve most likely they’ll have to go on aerosolized therapy afterward.
However, for patients with more extensive disease, Clazon Martin CT scan (on right), such as the patient whose CT scan saw his disease was so extensive that the polyps were causing his Left eye to bulge out, oral or intravenous antifungals may be necessary. This should not be taken lightly and should be managed by someone such as an infectious disease specialist to be done safely. Once these more severe cases improve most likely they’ll have to go on aerosolized therapy afterward.
Allergic Fungal Sinusitis is a complex disease that needs to be understood better. As with this as in all other cases of chronic sinusitis, each case must be addressed in an individual manner and treatment needs to be tailored to the individual.