Is it a Pseudomonas Sinus Infection? Let’s take a look
A patient came to see me recently who I had treated for refractory Stenotrophomonas maltophilia sinusitis some twelve years ago. Since that time, she had been doing okay, but over the last 2-3 years, her sinuses had become much more bothersome. On several occasions, sinus cultures revealed Pseudomonas aeruginosa in the nose, sensitive to the Cipro she was prescribed, but the patient did not experience any relief and the infection persisted.
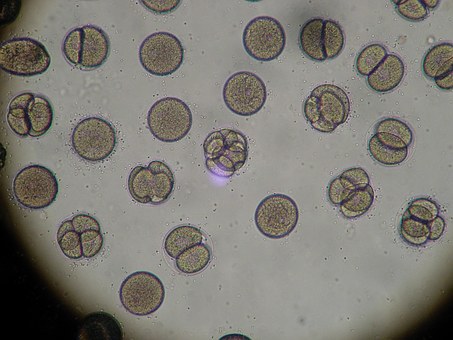
On physical exam, the nasal mucosa was found to be erythematous and swollen with purulent secretions visible. The rest of the physical exam was non-contributory. Based on these findings, my initial concern was allergic fungal sinusitis and a DNA analysis was performed.
To my surprise, no fungus was detected, but there were some interesting findings nonetheless from the DNA analysis. Pseudomonas was a minor player in the biofilm of this patient in particular. It turned out that a majority of organisms of the biofilm were anaerobes and the true pathogens for the patient’s persistent infection.
Why were cultures growing Pseudomonas Aerunginosa in the sinus?
The reason is that anaerobes are fastidious organisms and don’t grow well on conventional, commercial medium. So even a small amount of organisms like Pseudomonas are able to dominate and proliferate on the media and appear to be the causative agent in the infection.
This problem is then worsened by the fact that the selective pressure of the Cipro allows the anaerobes to grow unimpeded and create further damage to the sinus cavities. In addition, the biofilm is allowed to become more extensive, raising the potential for the exchange of genetic material between organisms increasing the virulence factors of the bacteria. Also, it probably was the biofilm that protected the Pseudomonas from being completely eradicated because of the glycocalyx that has the potential to shield the organisms from the effects of antibiotics.
Treating a Pseudomonas Sinus Infection
The patient was switched to clindamycin orally and is doing better. Her long-term management will include topical antibiotics that cover both anaerobes and Pseudomonas.
This case is a perfect representation of how routine cultures may not represent what are the actual pathogens in chronic infections, especially when dealing with chronic sinusitis. Not only does DNA analysis help in identifying the true pathogens, but allows for more precise antibiotic regimens to treat the infection. This will allow for better antibiotic stewardship by lessening the use of broad-spectrum antibiotics in chronic infections, which will reduce the rate of resistance by targeting the actual offending agents and not what grows the best on regular media, leading to multiple courses of antibiotics that are missing the mark.