As has been discussed often in the past, here at this blog chronic rhinosinusitis (CRS) is a very complex disease. It takes in both anatomical and physiological changes that bring about the disease state. Without adequate drainage of sinus cavities, secretions pool, causing the accumulation of fluid. Once this occurs, accumulated mucosal secretions act as a media for bacteria that normally colonize the sinus cavities. Once this occurs, the bacteria proliferate which leads to an infectious state.
In addition, there are physiological risk factors that can also contribute to chronic sinusitis. These include: Gastro-Esophageal Reflux Disease or GERD, Immunoglobulin deficiencies, allergic rhinitis and allergic fungal sinusitis. These risk factors allow for mucosal damage to the sinus cavities. When this occurs, it allows bacteria that are normal colonizers of the sinus cavities to obtain a foothold in the submucosa. This then leads to an infection in the mucoperiosteal layer, requiring higher concentration of antibiotics for longer periods of time. In most instances, chronic sinusitis usually involves either one or several of the above risk factors that have been a talked about, including anatomical changes.
It is this complexity that has made chronic sinusitis one of the most challenging chronic diseases in the United States today. Unfortunately, there are other concerns associated with chronic sinusitis that are not related to the above subjects that have been discussed. This includes the microbial makeup of the organisms that are involved in chronic sinusitis. Recent studies done by DNA sequencing have shown some very interesting results.
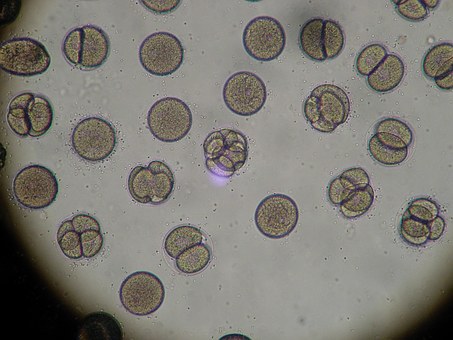
In the study, which evaluated approximately 80,000 ENT samples, 850 species were shown to have dominant roles in a sample at any given time. Interestingly enough, only in a small percentage of samples, the dominant species are commonly described as CRS pathogens:
- Staph aureus: 11%
- Pseudomonas aeruginosa: 8%
- Haemophilus influenzae: 4%
- Anaerobes: 45%, dominant in 12%
- Fungi: 22%
According to the American Thoracic Society’s Proceedings from 2010, the majority microbes involved in CRS are S. aureus and anaerobes, as seen from DNA sequencing, S. aureus was only seen in 11% of the samples examined. Anaerobes did dominate the spectrum as pathogens involved in CRS. What was more surprising was that over 20% of the samples had fungus present. Again, according to the American Thoracic Society, fungal sinusitis is only seen in patients severely immunocompromised, such as those suffering with neutropenia.
In addressing anaerobes associated with CRS, there is concern about antibiotic resistance detection by conventional methods. Anaerobes do not grow well on conventional media, making standard inhibition techniques to determine resistance inaccurate. DNA sequencing can allow for better detection of anaerobic resistance and allow for better choices in antibiotic coverage.
For years, many of us that work extensively with CRS have known about the relationship between CRS and fungus. Unfortunately, there are many who disagree with fungus being a major pathogen and contributor to CRS. Fungi such as Bipolaris, Alternaria, Curvularia and only a small amount due to Aspergillus, can cause recurrent sinusitis in normal hosts. Based on these findings, the importance of fungi in CRS can be understood and no longer be ignored, thanks to DNA sequencing.
CRS is one of the most common chronic diseases seen today. The cost annually to the United States is over $10 billion, affecting over 20 million patients. In order to do a better job of managing this disease, we need to have a better understanding of the microbial makeup involved in CRS. DNA sequencing will be of great help in moving forward with the management of CRS.