A 43 year old woman came to the office nine months ago with a recurrent history of chronic sinusitis over the last 7-8 years. The patient had recently gone through her second sinus surgery and it was perplexing to her ENT as she continued to have recurrent infections, despite having adequate drainage of the sinus cavities.
DNA sequencing of the patient demonstrated that she had a complex infection. Not only would staph aureus which turned out to be MRSA, but Enterobacter cloacae. The significance of finding Enterobacter cloacae in the sinus cavities is highly suggestive of a reflux component contributing to the patient’s recurrent sinus issues.
Physical exam showed that the patient had a neck circumference of 16 inches and macroglossia. When questioned about snoring, the patient admitted that she had woken herself up on several occasions snoring and that she would wake up several times a night. It appeared to the patient that her sinus congestion and post-nasal drip were worse first thing in the morning.
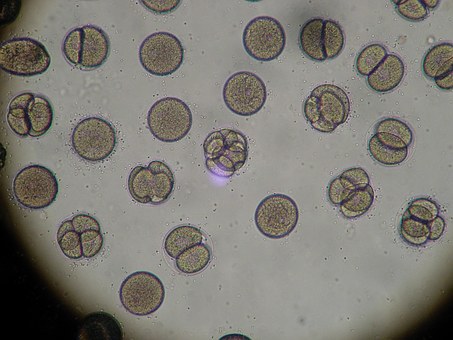
The patient had also been advised that she needed to be tested for allergies. She had gone through the allergy testing with her ENT and was found to be allergic to multiple pollens.
Due to the fact that the patient had failed multiple courses of oral antibiotics, the patient was placed on intravenous antibiotics which included Daptomycin and Invanz. DNA sequencing did show medicine resistance but no carbapenem resistance.
Besides antibiotic therapy, the patient began allergy immunotherapy. In addition, she underwent a home sleep study and was found to have moderate to severe obstructive sleep apnea. She was provided with a C pap and has been compliant with it since the beginning. Once the patient completed intravenous antibiotic therapy approximately six months ago, the patient has not had any recurrent sinus infections.
This is another example of the importance of managing underlying medical problems to improve the management of chronic sinusitis. For this patient in particular, reflux was the driving force behind her recurrence of sinus infections. It is important for patients with reflux, even if it may appear to be silent, to adhere to the lifestyle changes that can be extremely important in minimizing reflux, especially nocturnal reflux. These include avoiding both caffeine products and alcohol at night, plus not eating for at least three hours before bed. Patients that adhere to these lifestyle changes usually find much better management of their nocturnal reflux. Despite lifestyle changes, if a patient has underlying sleep apnea like this patient – in particular, obstructive sleep apnea, this can be a contributing factor to exacerbating nocturnal reflux.
The mechanism behind worsening reflux due to obstructive sleep apnea is not well understood, but the most common theory is OSA creates negative pressure in the chest cavity, compared to the abdominal cavity, and siphons gastric secretions back up the esophagus into the throat , sinus and lungs. By addressing the obstructive sleep apnea, this process is minimized, thereby alleviating a risk factor for reflux – especially nocturnal reflux.
In addition, patients with environmental allergies have a tendency to also have worse reflux. This is due to histamine release due to the allergies. In our stomachs we have histamine receptors known as H2 receptors. When stimulated, they produce more acid. It is not unusual to see patients with pollen allergies have worsening symptoms of sinusitis and bronchitis, along with laryngitis, due to worsening reflux. In these situations, H2 blockers such as Pepcid AC work very well.
Here is another example of the importance of managing underlying medical problems in patients with chronic sinusitis. It is extremely important to identify these risk factors in each individual to see how they can be managed in order to improve the overall outcome of patients with recurrent chronic sinusitis. By addressing these risk factors, we minimize the necessity for antibiotic therapy, thereby reducing the risk of developing resistant bacteria in these patients.