Interaction Between Fungus & Bacteria
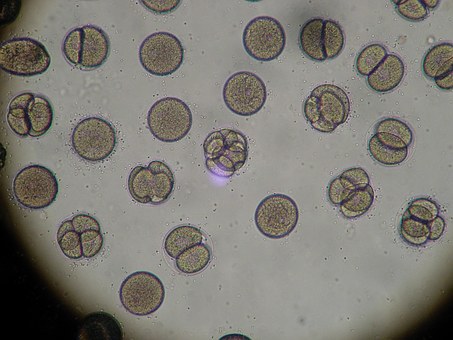
A Case of Scedosporium apiospermum
by Dr. Andrew Pugliese
A 64 year old otherwise healthy woman underwent a nasal septoplasty in April of this year and soon afterward developed a hematoma that progressed to an abscess. Despite multiple debridements and several courses of oral antibiotics, the abscess progressively worsened. Several cultures revealed only normal oropharyngeal flora. The last culture done showed Scedosporium apiospermum, a saprophytic fungus that has become increasingly involved in causing soft tissue infections in humans especially those who are immunocompromised or have some other underlying illness.
To learn more about fungus and sinusitis, check out this post.
It was decided because cartilage was involved, that the patient would be treated with intravenous (IV) voroniconazole along with ceftriaxone. The addition of ceftriaxone was for the secondary bacterial infection that most likely was there, due to the underlying fungal infection. The patient responded very well to treatment, and the regimen was discontinued after four weeks. However, there was a superficial infection that developed subsequently and the patient is now on clindamycin and doing well.
As already stated, the patient does not have any underlying illnesses, so why did such an infection occur? The answer is probably as complex as the infection itself. The lynchpin is that as we, as a species, continue to evolve, so will the diseases we will see and the infections that go along with it.
To learn more about the evolution of infection, check out this post.
In addition, though 64 is not considered old today by any stretch of the imagination, you have to be concerned that despite being healthy, how good was the blood flow to the nasal cartilage compared to a younger individual? Environmentally, the Southeast is notorious for mold, due to favorable weather patterns for mold. There is a lot of organic matter due to an abundance of vegetation, high humidity and no real winter to speak of.
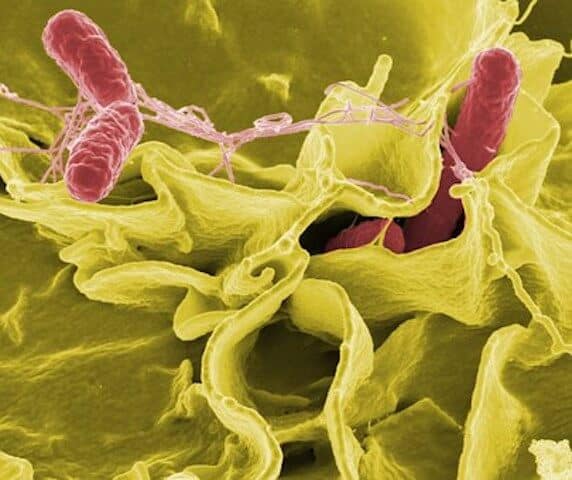
The critical concern, in cases like this, is the association between fungus and bacteria and the potential for increased virulence. Recent data has demonstrated that
The influences these interactions can be seen not only from a medical point of view but also commercially in the field of agriculture. Based on these findings, it is plausible that there may have been some exchange of genetic material between the Scedosporium and the “normal” oropharyngeal flora, increasing the virulence factor of the normal bacterial flora making it more pathogenic.
In this case, we got lucky, because in many instances, the fungus doesn’t routinely grow on culture media, but the wakeup call here is that we see more and more fungal infections which will continue to rise as time goes on. More complex patients will lead to more complex infections, and as we push the evolutionary envelope, there will be a push back by the organisms.